Featured Labs
Long Ping Victor Tse, Ph.D. Lab
Researching Virus-Host Interactions and Antiviral Development
The recurring emergence of animal coronaviruses (CoVs) and their ability to cross geographic and species barriers, exemplified by the COVID-19 pandemic, highlights the crucial importance of understanding the host pathways and viral factors involved in zoonotic transmission. Through genome-wide CRISPR screens, we aim to identify key host and immune factors that influence viral infection.
Our focus is on unraveling the molecular mechanisms underlying virus-host interactions. Leveraging this knowledge, we strive to develop effective antivirals that target both the virus directly and host factors. Our recent discovery of a viral host factor called PLAC8, essential for replicating emerging coronaviruses in human cells, has significantly advanced our understanding (Tse LV and Meganck RM et al. PNAS 2022). We are currently investigating how coronaviruses exploit the PLAC8 pathway for efficient replication.
Exploring viral Evolution and Vaccine Development Dengue virus (DENV) poses a significant global public health concern, causing millions of infections annually and potentially spreading even more due to factors such as global warming and increased mosquito populations. Overcoming the challenge of antibody-dependent enhancement (ADE) is critical for developing safe and effective DENV vaccines. Our laboratory employs directed evolution techniques to remove ADE epitopes from DENV vaccines (Tse LV et al. mBio 2022 and Meganck RM et al. bioRxiv 2023). By engineering vaccines that lack ADE epitopes, we aim to prevent the potential risk of ADE responses in vaccine recipients.
In summary, our research focuses on understanding virus-host interactions, developing antiviral strategies, and exploring vaccine approaches to combat emerging coronaviruses and mitigate the impact of dengue virus infections.
Follow @TseLabVirology on Twitter
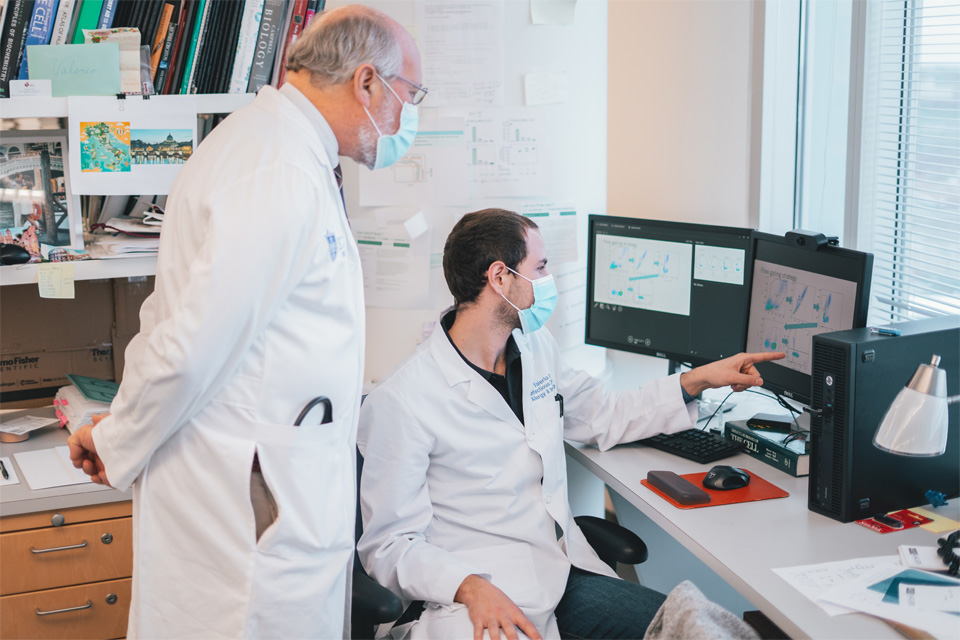
Dan Hoft, M.D., Ph.D., Lab
Daniel Hoft, M.D., Ph.D., focuses on developing vaccines against mucosally transmitted, intracellular pathogens in animal and human models. His lab was the first to report that CD4+ Th1 and not Th2 cells provide mucosal and systemic protection, indicating that coordinated mucosal/systemic immunity is achievable. His lab reported the first evidence that CD4+ Th17 cells provide potent helper effects for the induction of protective CD8+ T cells, implicating Th17 cells as important targets for vaccines against intracellular pathogens and cancer.
His group pioneered the use of immunoinformatics to develop T cell-targeting, “universal” vaccines to protect all human populations against future influenza pandemics. In addition to contributions in pre-clinical vaccinology, Hoft has conducted human trials to improve tuberculosis (TB) vaccines. Although BCG vaccines are available, protection is limited and better vaccines are urgently needed. Hoft’s clinical trials have tested whether mucosal, booster and/or novel recombinant vaccinations can enhance TB immunity. His lab was the first to demonstrate that human γ9δ2 T cells can provide TB protective memory responses, a paradigm shift providing new approaches for TB vaccination.
Furthermore, Hoft’s lab has identified new TB antigens that induce protective γ9δ2 T cells, now being studied in nonhuman primates. Hoft serves as Director of the Saint Louis University Center for Vaccine Development, which has received millions in NIH funding through contracts and awards, including a Vaccine & Treatment Evaluation Unit cooperative grant placing SLU among an elite group of top academic centers conducting phase I through III trials of novel vaccines for global protection against future pandemic challenges. Since the COVID-19 pandemic began, Hoft has led urgent vaccine trials, which continue to be ongoing, and is conducting new research focused on the development of universal pandemic coronavirus vaccines.
Valerio Rasi is an M.D./Ph.D. student (G5) originally from Italy. After graduating summa cum laude from the University of Florida with a degree in biochemistry, he joined the Saint Louis University M.D./Ph.D. program in 2015. He is finishing his Ph.D. in molecular microbiology and immunology under the mentorship of Daniel Hoft, M.D., Ph.D. Throughout his time at SLU, Rasi obtained the prestigious pre-doctoral (F30) fellowship from the National Institute of Health, which is funding his Ph.D. and the remaining portion of his M.D. His research focuses on understanding how a protein secreted by γ9δ2 T cells, Granzyme A, inhibits the intracellular replication of mycobacterium tuberculosis within human macrophages. Outside of research, he enjoys traveling, swimming and cooking.
Daniel Hawiger, M.D., Ph.D., Lab
Dendritic cells (DCs) have crucial roles in priming effector T cells, but DCs also have critical tolerogenic functions in the peripheral immune system, extending the maintenance of immune homeostasis and blocking autoimmune responses. However, broad tolerogenic functions of DCs, including induction of peripheral regulatory T cells (pTreg cells) could hamper protective immune responses against some pathogens and tumors. In contrast, an inadvertent activation of autoregressive T cells in the presence of pro-inflammatory stimuli could lead to autoimmunity. Therefore the maintenance of immune homeostasis by DCs requires specific mechanisms that actively adjust T cell functions to promote tolerance while preserving overall high plasticity of the immune responses.
(DCs with specialized tolerogenic functions are represented here as red flowers attracting naïve T cells depicted as green bees that can acquire regulatory functions, symbolized as purple halos. Trends in Immunology, 2017, Nov;38(11):793-804).
To clarify the mechanisms by which DCs govern T cell tolerance in the context of autoimmune disorders such as multiple sclerosis (MS) but also other immune responses, studies in my laboratory are focused on the roles of specialized subsets of DCs and their specific functions in tolerance as well as the relevant molecular mechanisms induced by such DCs in T cells. Our work has elucidated the functions of specific immunomodulatory pathways, cell signaling regulators and transcription factors that establish tolerogenic outcomes of the interactions between T cells and DCs.
Health Outcomes Research Ph.D.
The Health Outcomes Research Ph.D. program is housed in the Saint Louis University Department of Health and Clinical Outcomes Research and students partner with the Advanced Health Data (AHEAD) Institute.
The AHEAD team comprises faculty, researchers, staff, and doctoral students who are experts in statistics, medicine, public health, economics, program evaluation and research methodology to help improve patient and population health, advance healthcare quality, and decrease healthcare costs. Researchers utilize and develop data resources; novel analytic methods; predictive modeling; machine learning; and integrated, wearable health devices and will collaborate with national research networks.
The research conducted at the AHEAD Institute covers a variety of disciplines and topics, including epidemiology, health services, quality improvement, health outcomes, economics, social determinants of health, health disparities and geospatial intelligence. Current doctoral student projects include examining patterns of mental health treatment among people with Parkinson's disease, geospatial analysis of factors related to COVID-19 spread, and palliative care approaches in heart failure.
M.D./Ph.D. students training in the Department of Health and Clinical Outcomes Research have full access to the AHEAD institute, opportunities to collaborate with physicians throughout SLU and SSM, and graduate well-equipped for a career as a clinician-scientist, integrating clinical insight with research expertise.